Health, Medicine
Reimagining Medicine
Reimagining Medicine
by Alison Jones
Dr. Ray Barfield almost walked away from medicine. Now he wants to prevent doctor burnout – and to reshape pre-medical education.
Reimagining Medicine
by Alison Jones
Dr. Ray Barfield almost walked away from medicine. Now he wants to prevent doctor burnout – and to reshape pre-medical education.
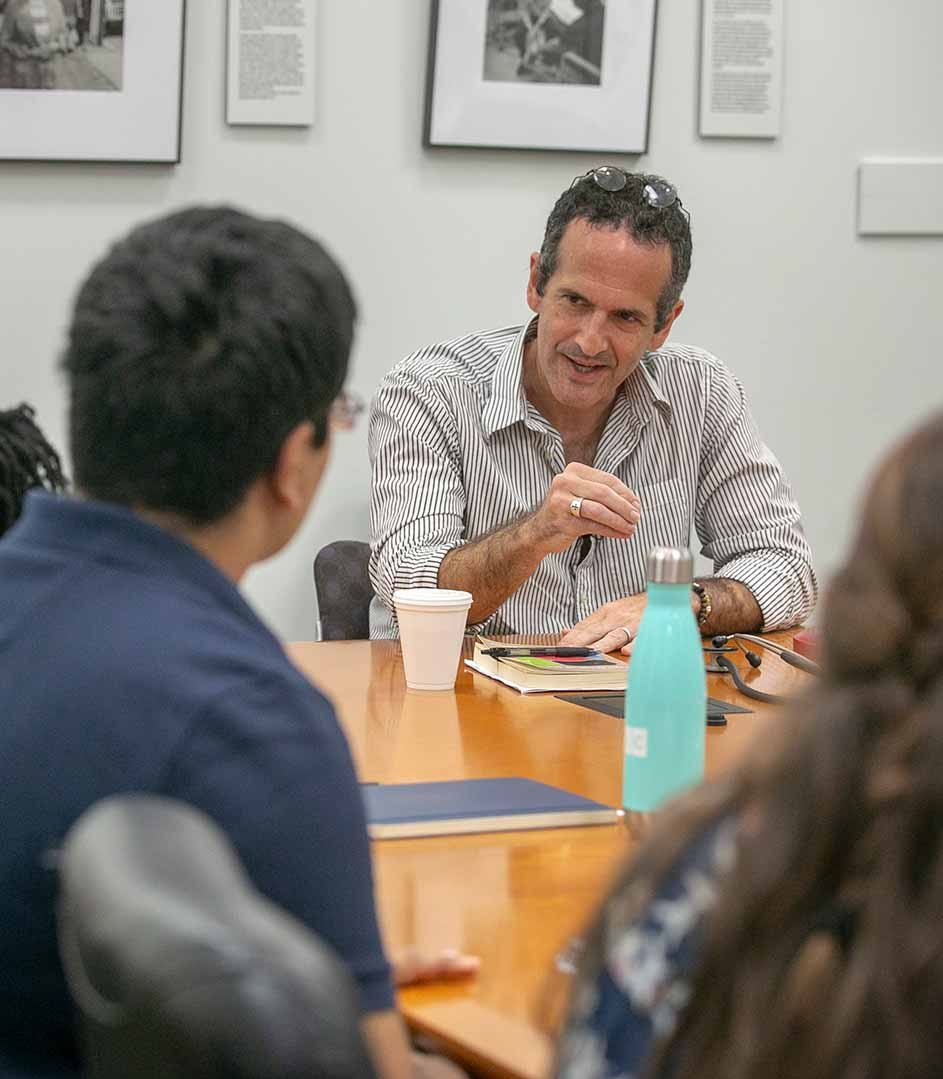
A few years after becoming a doctor, Ray Barfield faced a crisis.
He could handle the long hours and difficult decisions facing a pediatric oncologist. He felt confident in his mastery of biology and his growing diagnostic skills. Yet none of that helped when he sat down with a young mother to tell her the terrible news: There was nothing more he could do to save her 8-year-old daughter’s life.
“At that moment, I broke,” Barfield says. “I wasn’t sure I could keep on practicing medicine.”
Doctors’ days brim with such heartbreaking moments. But Barfield’s training hadn’t prepared him for the emotional demands of doctoring – for the human side of medicine.
So he started over, reinventing the way he approached his patients and his practice.
“I had to learn all these lessons the hard way,” says Barfield, who teaches pediatrics at Duke Medical School and Christian philosophy at Duke Divinity School. “I had very little instruction or mentorship around these kinds of topics and issues in my own training. I learned largely from failing and not being sure what happened.”
“I had to learn all these lessons the hard way... I learned largely from failing and not being sure what happened.”
– Ray Barfield
Now Barfield is sharing some of those lessons with Duke undergraduates who aspire to be doctors. His new pilot program, “Reimagining Medicine,” launched this summer with eight weeks of classes for 14 rising juniors and seniors. Barfield hopes it’s the start of a long-term effort to change how students prepare to be doctors.

Video: Ray Barfield describes the “Reimagining Medicine” program.
The curriculum wasn’t standard pre-med fare. No chemistry, biology or anatomy classes. Instead, students delved deeply into the arts and humanities through courses in topics such as improvisation, expressive writing, music and puppetry.
Ali Sloan, a junior neuroscience major, had doubts about some of the less traditional subjects at first.
“It challenged all of us to get out of our comfort zones,” Sloan said. “But in the end, it was an incredible opportunity for introspection and growth.”
Learning
How to Listen
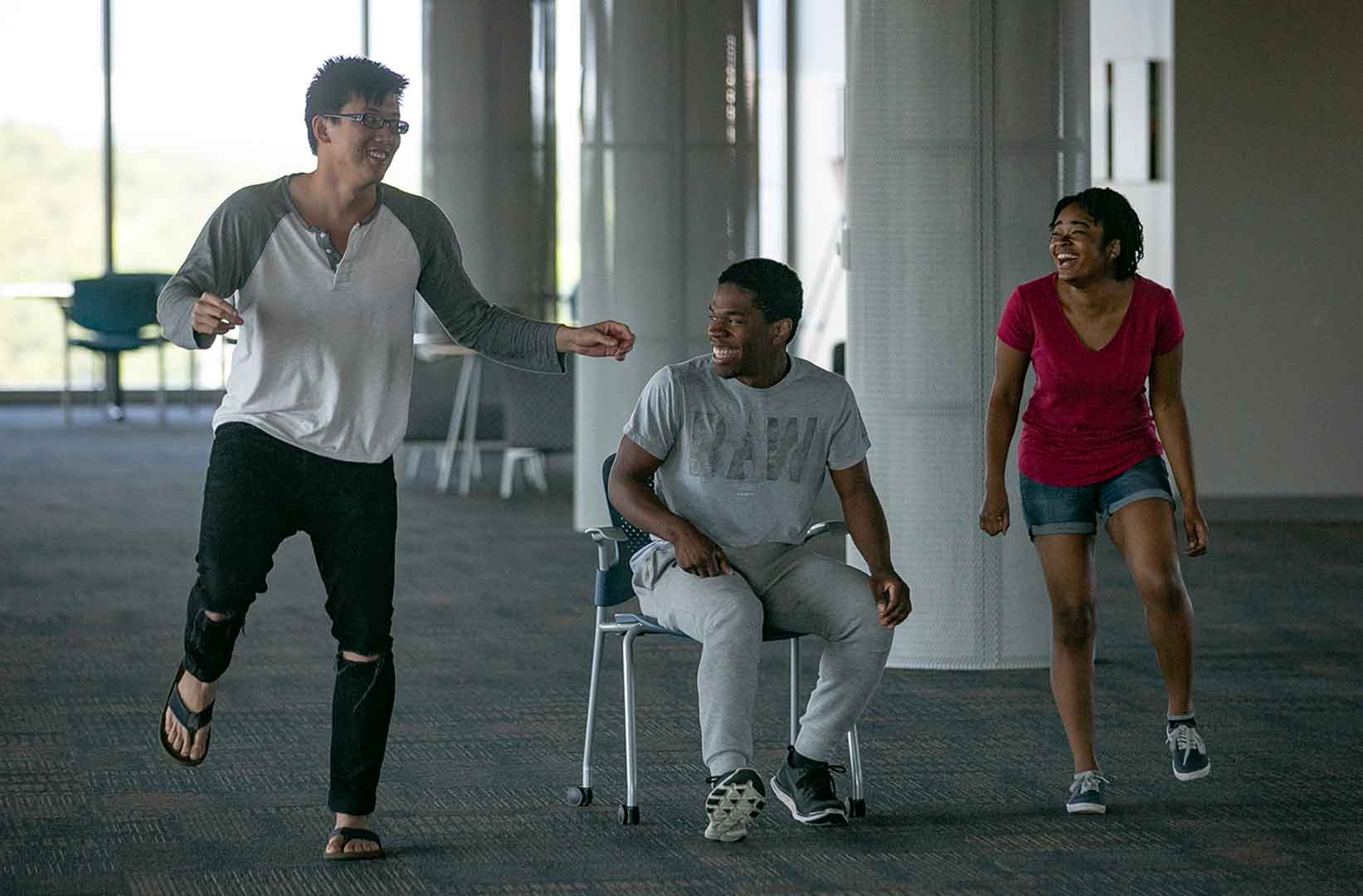
Students in the Reimagining Medicine program share a laugh during an exercise on musical improv.
Barfield and his colleagues think character is at the heart of good doctoring. In particular, they aim to nurture students’ empathy and imagination. Those, Barfield says, are precisely the tools doctors need – and often lack -- when they walk into a patient’s room and begin to listen to their stories.
“In medicine, conversations often go wrong because real communication and real listening isn’t happening,” Barfield says.
To strengthen their listening abilities, students worked with musicians and with actors skilled in improvisation. In improv, a student listens closely to a prompt from a partner and builds upon it. The conversation might go in any direction, which gives students practice in preparing for unpredictable situations – something they will face again and again as doctors.
Seeing
More Deeply
Students gather for a ‘Seeing Through Art’ session at the Nasher Museum of Art.
Doctors rely on many tools to diagnose. But none is more important than the ability to observe.
To nurture that talent, Reimagining Medicine took advantage of the visual arts. Duke dermatologist Lynn McKinley-Grant has found that visual art can sharpen doctors’ perceptive abilities, including helping them to see past the surface in dealing with patients. McKinley-Grant led students in observation exercises at the Nasher Museum of Art. Students also used drawing exercises to refine their powers of observation.

Nurturing Empathy
A student practices mindful listening next to the koi pond in Sarah P. Duke Gardens.
Every time a doctor walks into a patient’s room, he’s walking into someone’s story. And most often, that story is different from the doctor’s own.
It takes empathy to relate to someone much older or younger than oneself, and to connect with people of all races and social backgrounds. It takes, in other words, imaginative reach.
Reimagining Medicine sought to build students’ imaginative and empathetic capacity in several ways. The students shadowed not only doctors but also hospital chaplains, physical therapists, occupational therapists and hospice nurses.
With the help of puppeteer Marina Tsaplina, the students also worked with puppets to model treating different sorts of bodies.
They also practiced storytelling and expressive writing under the guidance of professional writers and storytellers.
Leah Rosen, a senior pre-med from Denver, appreciated the chance to think more deeply about what it is to be a doctor.
“There are so many intricacies about being a doctor that don’t necessarily get taught in pre-med courses,” Rosen said. “Someone may know how many carbons are in a benzene ring, but may not know why a patient is reacting to a diagnosis in an unexpected way, or how to give a family the support they need in that moment.”
“Doctors have to have scientific competency. But they also have to think in other ways – ways we’re not currently being taught.”
Preventing
Burnout
Students meditate during a mindfulness session in Sarah P. Duke Gardens.
Taken as a whole, Reimagining Medicine might be described as “care and feeding for future doctors’ souls.”
Right now, too many doctors are soul-sick, just as Barfield was a few years into the practice of medicine. And that, Barfield says, is bad for doctors and patients alike.

Video: Ray Barfield discusses the growing crisis of physician burnout.
“Physicians are in an important place in our society,” Barfield says. “We walk into their offices and tell them things we haven’t told our spouse. We undress in front of them. We let them give us chemicals that in any other setting would be poisonous. We let them cut pieces of our bodies off.
“They have an important role. We need them and we need them to be well. And right now many of them are not well.”
The numbers back him up. According to some studies, as many as 50 percent of practicing doctors report signs of burnout.
54%
54% of physicians report at least one symptom of burnout according to a 2014 Mayo Clinic study
“Physicians are in an important place in our society... We need them and we need them to be well. And right now many of them are not well.”
– Ray Barfield
Barfield hopes Reimagining Medicine is a step towards changing that. Plans are underway for a second offering of Reimagining Medicine next summer. Ultimately, Barfield would like to see it expand beyond a summer program.
And while the program’s approaches sound new, in one sense they are as old as medicine itself, Barfield says. It’s just that amid exploding technical and scientific advances, other time-honored aspects of being a doctor – the more human aspects, you might say – can get lost.
That emphasis on the human side of medicine resonated deeply with senior Akeim George, a premed from Nashville, Tennessee.
“The program showed me there are current medical professionals who see value in emphasizing the nonscientific aspects of medicine – and who see those as just as important as being a good scientist,” George said.
Barfield thinks those human elements of doctoring deserve to be center stage once again.
“Imagination, attention, presence, listening, mindfulness – these are not new to human beings. But they’re in danger of being excluded from the practice of modern medicine. They’re in danger of being forgotten,” Barfield says.
“We’ve called this ‘Reimagining Medicine.’ But we might have called it ‘Remembering Medicine.’ Great doctors have always known the importance of empathy, of close listening, of connecting with their patients.
“In an important sense, then, this is a return to what good medicine has always been about.”
Story by Alison Jones
Photos by Megan Mendenhall and Robert Zimmerman
Video by Julie Schoonmaker
Design by Jonathan Lee
Produced by University Communications
More about Reimagining Medicine:



